Kendra Pierre-Louis: For Scientific American’s Science Quickly, I’m Kendra Pierre-Louis, in for Rachel Feltman.
The birth of a child comes with a swirl of positive emotions: awe, joy, relief.
And yet, for many birthing parents, this postpartum period can also be accompanied by months—or even years—of debilitating depression. For some of these parents, traditional antidepressant meds like sertraline, better known as Zoloft, and fluoxetine, aka Prozac, have provided some relief. But many with postpartum depression have had little recourse. That may be starting to change.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Science journalist Marla Broadfoot looked into a new drug that might better treat people for whom relief has remained elusive.
Marla joins us today to talk about her recent story in Scientific American. Welcome, Marla.
Marla Broadfoot: Thanks for having me.
Pierre-Louis: At a very basic level can you explain what postpartum depression is?
Broadfoot: So at a basic level it is a mood disturbance. For a long time it was lumped in with all kinds of depression, like garden-variety depression, but only recently have people begun to realize—and researchers in particular—realize that [it] is its own entity.
Pierre-Louis: Mm-hmm.
Broadfoot: And part of that has to do with hormones and the big fluctuations in hormones during pregnancy and in the postpartum period and how the brain responds to that and how the brain responds in ways that maybe make you more vulnerable to mood disorders.
Pierre-Louis: And developing a mood disorder or some sort of a mental health issue post-pregnancy’s extremely common, correct?
Broadfoot: Yes, it’s very common. I mean, I think it’s 500,000 people in the U.S. develop postpartum [depression] every year, so that’s very common.
Pierre-Louis: And I know in the article you begin by talking about this woman named Kristina Leos. Can you tell me about her?
Broadfoot: Yeah, so Kristina is a 40-year-old nurse and mother of three, lives in Midlothian, Texas. And she told me that postpartum depression felt like a heavy cloud hanging over her. She felt like she was separated from her family and everything she loved. And it made her believe things that weren’t real. She thought that she was a burden to her family, that she was unfit to be a mother. At one point she actually [messaged] a friend and said, “Please come take my baby. I, I can’t take care of her. You could take care of her.” And she was, yeah, not afraid to die at one point. She even envisioned just driving off a bridge and thinking that would probably be the be—best outcome.
Pierre-Louis: Oh, wow.
Broadfoot: And because she was a nurse she kind of recognized the signs. And so she tried just about everything—she tried a bunch of different antidepressants and doses, and she would get better a little bit, and then she’d get worse again.
Pierre-Louis: Mm-hmm.
Broadfoot: And so she got to the point, it was, I think, nine months after the birth of her third child, Victoria, that her doctor said they were running out of options.
Pierre-Louis: Mm-hmm.
Broadfoot: And she gave her three options, which were ketamine, electroshock therapy …
Pierre-Louis: Mm-hmm.
Broadfoot: Or admission to a psychiatric hospital.
Pierre-Louis: Oh, wow.
Broadfoot: And at that point she already felt so much guilt from not really being there for her family that she couldn’t imagine—it was about Christmastime, too, and so she really didn’t wanna be away from them. And that’s where the story of zuranolone comes in.
Pierre-Louis: Yeah, what is zuranolone, and what makes it different from the antidepressants that she was taking?
Broadfoot: Yeah, so they act very differently on the brain, so there’s actually a lot that’s different about them. So the SSRIs are selective serotonin reuptake inhibitors, so essentially, they’re boosting kind of these feel-good brain chemicals.
Pierre-Louis: Mm-hmm.
Broadfoot: And that takes a while. It’s something that kinda has to build up in your system over time. So they typically take four to six weeks or longer, and maybe the first round won’t work, and so then you need to try a different one.
Pierre-Louis: Mm-hmm.
Broadfoot: Zuranolone is kind of a way of resetting your brain. So it is actually directly acting on the way that the brain circuitry works to help you calm down in times of stress. And so it—if you can target that, which zuranolone is targeting one—it’s called the GABA [gamma-aminobutyric acid] system.
Pierre-Louis: Mm-hmm.
Broadfoot: If it targets that, then you have a calming effect, and then it’s a more immediate effect. And they found that in clinical trials it worked within days. And the treatment typically takes a couple weeks to just fill the whole treatment, and then you typically don’t have symptoms come back after that.
Pierre-Louis: It seems like one of the differences between looking at postpartum depression versus sort of normal depression is normal depression is kind of, like, how your brain is, and postpartum is almost, like, pregnancy changes sort of the brain system and you’re trying to reset it.
Broadfoot: Yes.
Pierre-Louis: Is that …
Broadfoot: I think that’s a really good point. I mean, it, it is obviously very complicated. [Laughs.]
Pierre-Louis: [Laughs.]
Broadfoot: But yes, your brain—you know, one thing that people often talk about is, “Oh, it’s just hormones.” Like, anything that’s women’s health is “just hormones.” But hormones are actually a really big deal. And so during pregnancy—I think it’s the third trimester of pregnancy—these hormones like progesterone and allopregnanolone, which is a related hormone, they increase [to as much as] 100 times what they normally are during a typical menstrual cycle.
Pierre-Louis: Mm-hmm.
Broadfoot: And that’s all just reprogramming your brain, kind of remodeling it to prepare you for motherhood. And then at childbirth it just drops off precipitously. And in some women that makes them very vulnerable to mood disorders because their brain hasn’t kind of compensated, and zuranolone is kind of designed to offset that drop-off.
Pierre-Louis: Kind of related to that can you tell me about the, like, melancholic mouse model, and why that was so important in helping research into postpartum depression?
Broadfoot: This is one of those interesting examples of serendipity in science. So there’s this researcher named Jamie Maguire, and about 17 years ago, when she was a postdoc training, she was interested in a different condition—it was a condition called catamenial epilepsy, where your seizures get worse during certain times of the month, during the menstrual cycle.
Pierre-Louis: Mm-hmm.
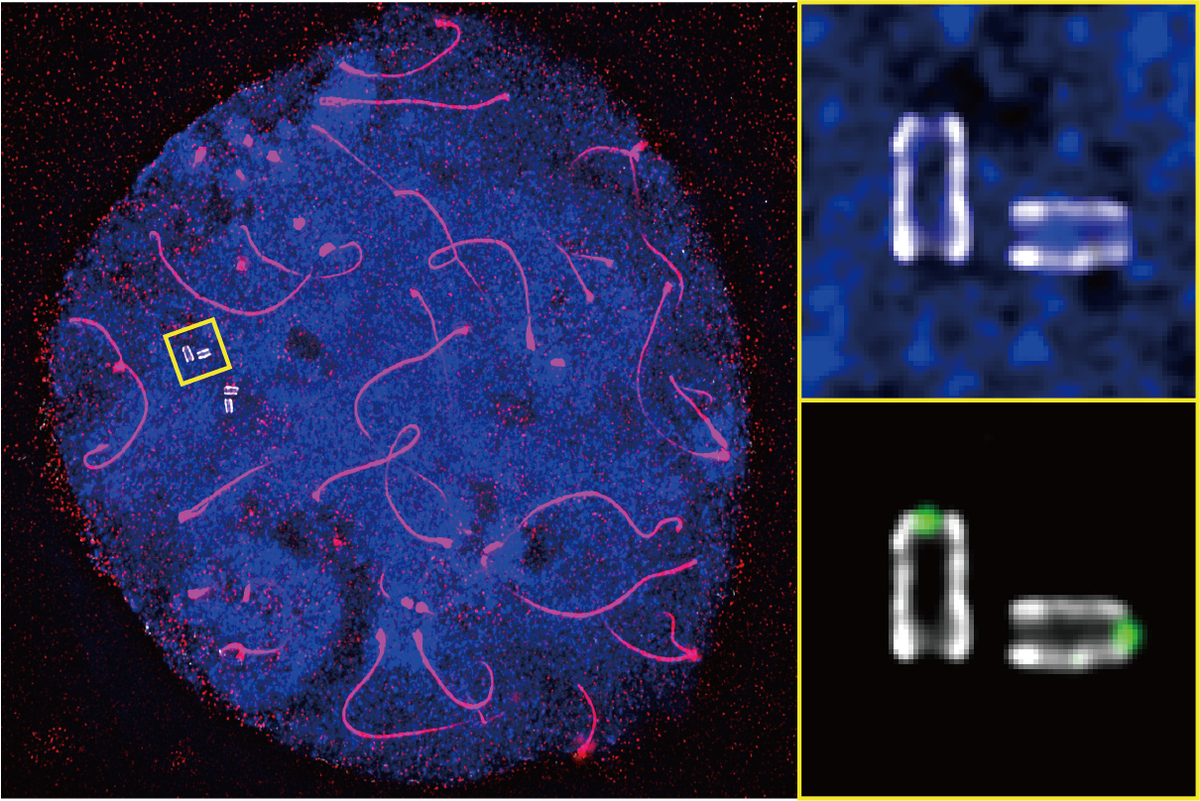
Broadfoot: And so she was interested in how neurosteroids, these brain steroids, might protect against these seizures. So she genetically engineered mice to kind of mess with and alter this neurosteroid signaling.
Pierre-Louis: Mm-hmm.
Broadfoot: And when she tried to breed these genetically engineered mice she found that they really weren’t breeding well, like, at all.
So they seemed perfectly normal until they gave birth.
Pierre-Louis: Mm-hmm.
Broadfoot: And then they acted a lot like [they had] depression, so they had symptoms like they weren’t really taking care of their pups; they weren’t building the, like, the little nests that you need for them.
Pierre-Louis: Mm-hmm.
Broadfoot: And so when, then, she gave them a compound that restored their ability to react to neurosteroid signals they behaved just as mouse mothers should. And that was the first time that there was really a kind of a direct connection between these brain steroids and postpartum depression.
Pierre-Louis: Zuranolone is potentially game-changing for many people, but there are some limitations around access, cost and, and effectiveness. Can you tell the listeners about it, about these caveats?
Broadfoot: Yeah, so it is—you know, like you said, it works remarkably well, and it’s fast-acting. So in clinical trials they found that about 60 percent of people who took it …
Pierre-Louis: Mm-hmm.
Broadfoot: Had a meaningful reduction of depression. And 60 percent might not seem like a lot, but then when you compare that to traditional antidepressants, those only work about half the time.
But the side effects are very real, so there’s dizziness, sleepiness, nausea.
Pierre-Louis: Mm-hmm.
Broadfoot: And because of that, you know, that’s prompted about 16 percent of women who take it to reduce the dose, and then about 4 percent just stop taking it altogether—the symptoms are just too much.
Pierre-Louis: Mm-hmm.
Broadfeet: And in addition to that there are issues with cost and access. So the drug costs nearly $16,000, and that’s for a two-week treatment. But then at the end of two weeks, as I said before, [for most people] the treatment is over, it’s done because it’s a reset.
And it is covered by Medicaid and most health insurance companies, though some states require patients and providers to jump through a few hoops. Like my state of North Carolina, for instance, you have to show that you’ve tried and failed other antidepressants before you can try zuranolone.
Pierre-Louis: Mm-hmm.
Broadfoot: And then on top of that you’ve got all the other barriers that women, particularly women of color or people in rural areas, face as far as financial burdens or access to providers.
Pierre-Louis: I believe you mentioned in the piece that even getting diagnosed with postpartum depression can be really difficult.
Broadfoot: Yeah, I mean, I think it’s less than half of women who show symptoms of postpartum depression are actually diagnosed with the disease, and even less than them get effective treatment.
Pierre-Louis: Why is there such a big gap for something that is so debilitating?
Broadfoot: Yeah, I think that’s a really good question. I mean, I think—one thing that I found with Kristina is that even though she—she’s a neonatal intensive care nurse, so she sees women, many of whom are expressing symptoms, and when you’re in it as an individual it’s really hard to recognize it. And she is even having a hard time recognizing that she was depressed.
Pierre-Louis: Mm-hmm.
Broadfoot: And it also kind of conflicts with all these societal expectations about what it is to be a mother and how you need to be happy about it. It’s supposed to be the best time of your life, but yet you feel this way.
And I think it often gets conflated with “baby blues.”
Pierre-Louis: Mm-hmm.
Broadfoot: Which is hormonal, but it’s often crying spells and mood swings that typically resolve after a couple weeks. But with this it is much deeper and darker and longer-lasting. And I mean, some women have it—I, I mean, there are cases that have lasted for 11 years.
Pierre-Louis: Oh, wow.
Broadfoot: So I think that it’s just underrecognized and underappreciated. But I think it’s from both sides: it’s from the stigma of it and then also just a lack of ways to look for it in the clinic.
Pierre-Louis: It’s kind of funny, too, if you think about it because there are all of these sort of negative stereotypes associated with women and menstruation and, like, “her time of the month,” but then we treat something as big and significant and hormone-shifting, as you noted, as pregnancy, and we’re like, “Oh, you’ll just bounce back.”
Broadfoot: Mm-hmm. Well, I think it goes to the—also that, you know, you, you have pretty intense treatment until the baby’s born, and then all of a sudden the baby gets all the treatment, and the mother is kind of like, “Okay, you did your job.”
And that’s where one of the clinicians I spoke to said that she really tries to start the conversation early, to make people aware that this is something that might happen and try to identify those that might be at higher risk and then be able to treat them after the fact. Because I do think the focus is so much on the baby at that point and, and not the mother, even though the mother could be going through something very significant.
Pierre-Louis: What conversations do you hope this piece sparks that weren’t happening before?
Broadfoot: I really hope that it reframes postpartum depression as not an inevitable emotional struggle but a treatable condition with clear roots in the brain and that it can kind of reduce the stigma that this is something that people can identify and treat. So I want women to realize it’s not their fault and that there is help and that there are treatments out there, and they’re transparent about how they’re feeling because it’s not something they have to bear alone.
Pierre-Louis: Given that, and given that you’ve covered a lot of science and health topics, is that partly why you think this story is so important right—and urgent to tell right now, because there are treatments, there are things we can do about this?
Broadfoot: Yeah, I think there was, like, two things that excited me most about this story, me as a former scientist. It’s a story of how an investment in basic research reaped big rewards—and it was much later. I mean, this discovery of allopregnanolone, which is pretty much the hormone that this treatment is based on, I mean, a lot of that research was done in the ’80s.
Pierre-Louis: Mm-hmm.
Broadfoot: And it’s basic research that I’m not sure in the current climate would be funded. So it shows a positive impact of something that was started quite some time ago.
The basic research side of it excites me, but then also as, as you mentioned, the women’s health side of it. I think it’s an area that has always been underfunded and understudied and underrecognized as being so important, but postpartum depression impacts the family and impacts the child. Then it can have intergenerational impacts.
Pierre-Louis: Mm-hmm.
Broadfoot: We’re not just talking about the mom; we’re talking about the family. So I think it’s very important. And I think it’s wonderful that we have something now that we can talk about that’s positive, not just about the biology and “oh, well, this is the way it is” but “here’s the biology, and this is a path forward.”
Pierre-Louis: It is really wonderful in this moment to have hope and to have real, effective treatments. And that seems like a really lovely note to end this on. Thank you so much for taking the time to speak with us today.
Broadfoot: Well, thanks for having me. It was really wonderful.
Pierre-Louis: That’s all for today’s episode. Tune in on Monday for our science news roundup.
Science Quickly is produced by me, Kendra Pierre-Louis, along with Fonda Mwangi and Jeff DelViscio. Shayna Posses and Aaron Shattuck fact-check our show. Our theme music was composed by Dominic Smith. Subscribe to Scientific American for more up-to-date and in-depth science news.
For Scientific American, this is Kendra Pierre-Louis. See you next week!